The History of Gynecological Ultrasound: From Early Innovation to Modern Excellence
Introduction
Ultrasound has become an indispensable tool in women’s health, empowering clinicians with the ability to visualize, diagnose, and monitor gynecological and obstetric conditions with remarkable accuracy. While today’s systems are defined by high-resolution 2D and 3D/4D imaging, artificial intelligence (AI)-assisted workflows, and seamless integration into electronic medical records, the journey of gynecological ultrasound spans nearly a century of innovation.
In this article, we explore the history of gynecological ultrasound—from its experimental beginnings in the 20th century to the advanced, specialty-tailored solutions now shaping modern clinical practice.
The Origins: Ultrasound Enters Medicine
The science of ultrasound traces back to the late 18th and early 19th centuries, when researchers discovered the phenomenon of sound waves traveling through different media. But it wasn’t until the early 20th century that ultrasound’s medical applications began to take shape.
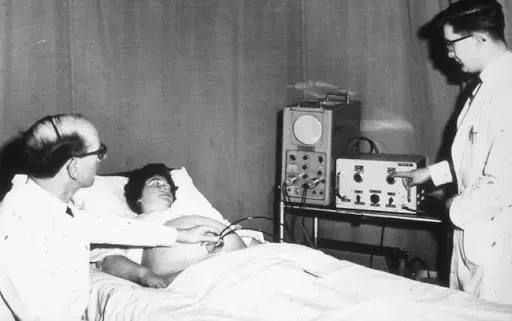
During World War II, sonar technology was developed to detect submarines. After the war, pioneers in medicine recognized that similar principles could be applied to visualize structures inside the human body. By the 1940s and 1950s, early ultrasound machines began to emerge, though they were bulky, slow, and limited in clarity.
The first clinical uses of ultrasound in obstetrics and gynecology came in the 1950s, when physicians sought safer alternatives to X-ray imaging for pregnancy care. Scottish obstetrician Ian Donald is often credited as the father of obstetric ultrasound. His groundbreaking work in the late 1950s demonstrated that sound waves could safely differentiate between various types of tissues, paving the way for routine fetal and gynecological imaging.
The 1960s–1970s: Ultrasound Becomes a Clinical Tool
By the 1960s, ultrasound technology was moving out of the laboratory and into hospitals. A-mode (amplitude) and B-mode (brightness) imaging gave clinicians their first consistent real-time views of pelvic anatomy. This was revolutionary for gynecology, as physicians could noninvasively assess reproductive organs, detect abnormalities, and monitor early pregnancies without radiation exposure.
In the 1970s, real-time ultrasound systems began to replace static images, offering dynamic visualization of moving structures such as the fetal heartbeat. Transabdominal scanning was standard, requiring a full bladder for better acoustic windows. While image resolution was still modest, gynecological ultrasound had established itself as a safe, essential diagnostic tool.
The 1980s: The Rise of Transvaginal Ultrasound
Perhaps the most transformative advance for gynecology came in the 1980s with the development of transvaginal ultrasound probes. By positioning the transducer closer to the uterus and ovaries, clinicians achieved higher-resolution images with greater detail than ever before.
This innovation revolutionized gynecological imaging:
- Early pregnancy assessment became more accurate, allowing clinicians to confirm viability and detect ectopic pregnancies sooner.
- Reproductive medicine advanced significantly, as transvaginal ultrasound enabled precise monitoring of follicular development and guided assisted reproductive procedures.
- Gynecological pathology detection improved, with enhanced ability to evaluate ovarian cysts, uterine fibroids, endometrial thickness, and pelvic masses.
Transvaginal ultrasound remains a cornerstone of gynecological practice today, delivering clarity and confidence for both routine and complex cases.
The 1990s: Digital Imaging and Doppler Advancements
By the 1990s, ultrasound entered the digital age. Enhanced computing power allowed systems to deliver sharper, more detailed images while storing and transmitting data with greater efficiency.
For gynecology, the introduction of color Doppler and power Doppler provided a new dimension: the ability to assess blood flow within pelvic organs. This had a major impact on the evaluation of ovarian and uterine masses, endometrial pathology, and infertility assessments.
Three-dimensional ultrasound also emerged during this era, giving clinicians the ability to reconstruct and analyze the uterus, ovaries, and pelvic floor in ways never before possible. For the first time, gynecological imaging could combine anatomical precision with spatial awareness, helping with surgical planning and diagnosis of congenital anomalies.
The 2000s: 3D/4D Imaging and Workflow Integration
As ultrasound entered the new millennium, innovations accelerated. 3D ultrasound became more widely available and clinically validated. In obstetrics, 4D (real-time 3D) imaging captured public attention with lifelike fetal images, but in gynecology, its impact was just as profound.
Clinicians gained powerful tools for:
- Uterine assessment
– Accurately diagnosing congenital anomalies like septate uterus.
- Reproductive medicine – Evaluating endometrial receptivity and follicular development with greater precision.
- Minimally invasive gynecology – Planning surgical approaches for fibroids, polyps, and adhesions.
At the same time, ultrasound systems became more compact, user-friendly, and integrated with hospital IT infrastructure. DICOM connectivity enabled seamless data sharing with PACS and EMR systems, supporting more efficient workflows.
Today: AI, Portability, and Specialty-Driven Imaging
Modern gynecological ultrasound has advanced far beyond its early pioneers could have imagined. Today’s systems combine exceptional image resolution with intelligent automation, improving both diagnostic confidence and clinical efficiency.
Key innovations shaping gynecological ultrasound today:
- Artificial Intelligence (AI) and automation – Smart measurement tools, automated follicle counts, and advanced image optimization reduce repetitive tasks and standardize results across users.
- Enhanced ergonomics – Slim, lightweight consoles and portable systems like Philips, Alpinion, and Mindray deliver high-end performance in space-conscious clinical environments.
- Portability and point-of-care flexibility
– Compact, battery-powered units allow imaging at the bedside, in ambulatory clinics, or across multiple practice rooms.
- Advanced Doppler technologies – Provide sensitive vascular assessment for tumors, endometrial evaluation, and reproductive medicine.
- 3D/4D refinement – High-definition rendering enables detailed uterine and ovarian assessment, assisting in both diagnosis and treatment planning.
- Specialty-tailored systems – Purpose-built solutions for OB/GYN and reproductive medicine deliver optimized presets, intuitive workflows, and gynecology-specific applications.
At Preferred Medical, we see firsthand how these innovations empower OB/GYNs, reproductive specialists, and women’s health providers to elevate patient care while improving operational efficiency.

The Future of Gynecological Ultrasound
Looking ahead, gynecological ultrasound will continue evolving in ways that enhance both clinical outcomes and patient experience. Emerging technologies such as AI-driven decision support, elastography for tissue characterization, and cloud-based imaging platforms promise to make ultrasound even more powerful and accessible.
For women’s health providers, the future will bring systems that not only produce clearer images but also act as intelligent clinical partners—streamlining workflows, integrating seamlessly with practice management, and delivering actionable insights in real time.
Conclusion: A Legacy of Innovation, A Future of Possibility
From its experimental roots in the 1950s to today’s AI-enhanced, specialty-driven imaging platforms, gynecological ultrasound has continually redefined what is possible in women’s healthcare. Each technological leap—from transvaginal imaging to Doppler, 3D/4D, and now AI—has empowered clinicians to deliver safer, more accurate, and more personalized care.
At Preferred Medical, we are proud to support providers with the latest in ultrasound innovation—combining world-class imaging systems from Philips, Alpinion, and Mindray with expert consultation, turnkey installation, personalized training, and long-term service support.
Ultrasound’s story in gynecology is one of progress, partnership, and patient-centered innovation—and its next chapter is only just beginning.

Leading Women’s Health Providers in Houston, TX: Advancing Imaging Innovation Across Southeast Texas